PGT-A & PGD Testing
Preimplantation Genetic Testing (PGT) encompasses a vital realm of reproductive medicine, offering comprehensive evaluation and screening for genetic anomalies in embryos before implantation. Two primary methodologies stand out: Preimplantation Genetic Screening (PGS) and Preimplantation Genetic Diagnosis (PGD). Both PGS and PGD represent sophisticated techniques aimed at ensuring the health and viability of embryos before they are transferred to the uterus, with the ultimate goal of fostering the birth of a healthy baby.PGS, referred to as Preimplantation Genetic Testing for Aneuploidies (PGT-A), focuses on detecting chromosomal abnormalities within embryos. This meticulous screening process involves analyzing the embryo’s chromosomal makeup to identify deviations from the typical number of chromosomes, thereby reducing the risk of implanting embryos prone to genetic disorders or developmental abnormalities.
On the other hand, PGD offers a deeper level of genetic scrutiny, targeting specific genetic mutations or disorders that may be inherited from the parents. Through PGD, potential genetic defects responsible for diseases such as cystic fibrosis, Huntington’s disease, or sickle cell anemia can be identified with remarkable precision. This personalized approach enables prospective parents to make informed decisions regarding embryo selection and implantation, thus significantly increasing the chances of a successful pregnancy and the birth of a healthy child.
carrier screening
A prevalent cause for unsuccessful embryo transfers leading to non-pregnancy stems from aberrant embryo genetics. Carrier screening is a pivotal diagnostic tool in evaluating genetic risks to a patient or couple’s prospective offspring, especially those not discernible solely through personal or familial medical history. Carrier screening is instrumental in identifying recessive disorders, wherein both gene copies must be impaired for an individual to manifest symptoms. This screening method detects potential genetic predispositions that may not manifest in the carriers but could be transmitted to future generations, enabling informed decision-making regarding reproductive choices and family planning strategies.
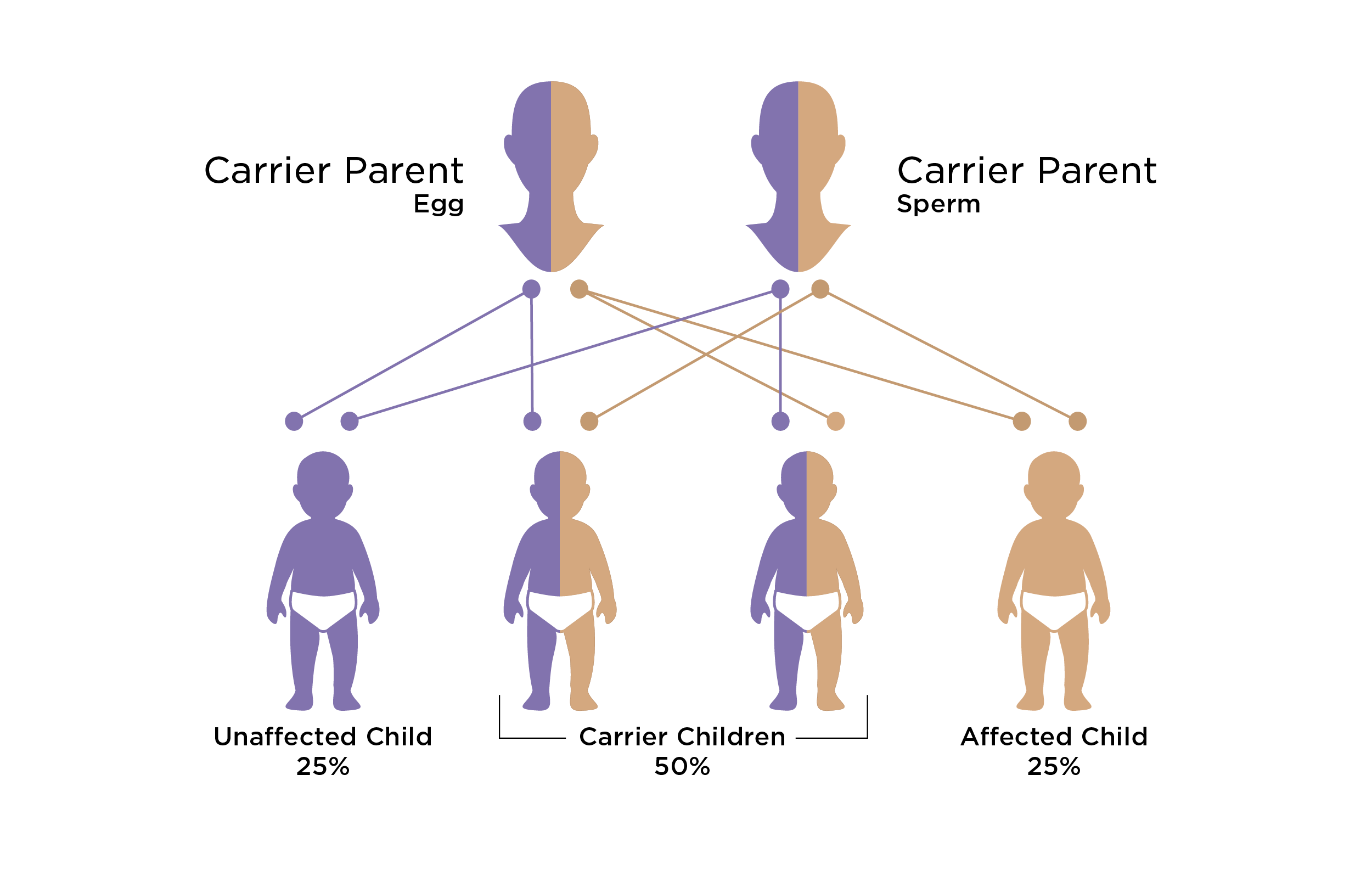
genetic conditions
In certain instances, both partners within a couple may harbor recessive genetic conditions, such as cystic fibrosis or sickle cell anemia. Carrier screening serves as a fundamental protocol, often encompassing the examination of prevalent X-linked conditions exclusive to individuals with two X chromosomes, such as Fragile X syndrome. Being a carrier of a genetic condition is expected, with many individuals carrying one or more recessive conditions without exhibiting any symptoms. However, when both partners are carriers of the same condition, the likelihood of passing the genetic disease to their offspring increases, reaching up to 25%. This underscores the importance of comprehensive carrier screening in elucidating potential genetic risks and facilitating informed reproductive decisions to mitigate the probability of hereditary disorders in future generations.

PGT testing
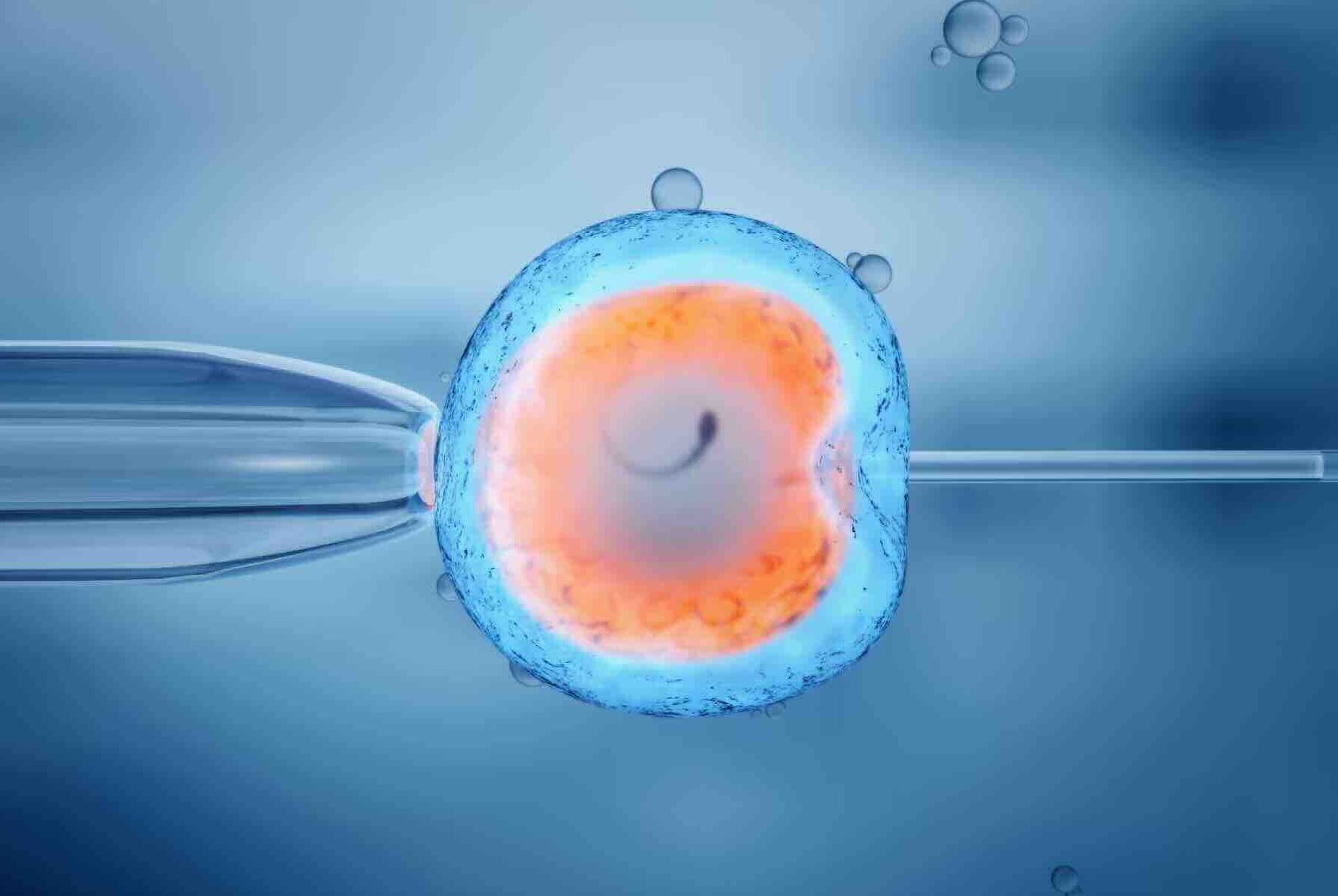
In cases where both individuals in a couple are identified as carriers of the same disease or when a female is a carrier for an X-linked disorder, in vitro fertilization (IVF) coupled with preimplantation genetic testing (PGT) offers a viable solution. This advanced reproductive technique allows for the screening of embryos before implantation, ensuring that only unaffected embryos are selected for transfer into the uterus, thus mitigating the risk of passing on the genetic disorder. By leveraging PGT, prospective parents can make informed decisions regarding embryo selection, optimizing the chances of a successful pregnancy while minimizing the likelihood of transmitting genetic conditions to offspring.
Assessment
Even if a couple opts for IVF without Preimplantation Genetic Testing (PGT), there are essential considerations to remember. Additional prenatal testing may be advisable; sometimes, preparing a specialized pediatric care team for postpartum needs is recommended.
Carrier screening is crucial in assessing genetic risks that may not be apparent from personal or family medical history alone. These screenings specifically target recessive disorders, where both gene copies must be affected for symptoms to manifest. By identifying carrier status, couples can make informed decisions about their reproductive choices and plan accordingly for the health and well-being of their future child.

PGT-Aneuploidy (PGT-A)
PGT-A analyzes embryo cells to determine if there is an average number of chromosomes. An unequal division of sperm or egg cells can result in an embryo having too few or too many chromosomes. Most people have 46 chromosomes because they inherit 23 chromosomes from each parent. If an embryo or a cell is missing a chromosome or has an extra one, it is called aneuploidy. Monosomy is a missing chromosome, and trisomy is an extra chromosome. A child can only survive one type of monosomy, Turner syndrome, which is the absence of one of the X chromosomes. Trisomy of chromosome pairs can sometimes result in a live birth, Down syndrome, also called trisomy 21 (an extra chromosome in average pair # 21), Turner syndrome (trisomy 18), and Patau syndrome (trisomy 13). Down syndrome affects 1 in 700 babies, according to the Centers for Disease Control and Prevention. Aneuploidy is one of the most significant causes of failed implantation for pregnancy and miscarriage, as well as an essential cause of congenital disabilities in children.
PGT-Monogenic Conditions (PGT-M)
Monogenic disorders are genetic disorders caused by a specific gene’s pathogenic variants (or changes). Preimplantation Genetic Testing for Monogenic Conditions (PGT-M), formerly known as Preimplantation Genetic Diagnosis (PGD), is utilized in situations with a known risk of a specific genetic disorder in the family. This knowledge can come from a known family or personal medical history, preconception/prenatal carrier screening, and previous genetic testing. The goal of PGT-M is to identify embryos free of the inherited condition for transfer. Preparing for PGT-M typically requires several months before a PGT lab is ready to analyze samples. This is because PGT-M involves the creation of a custom test for the family (sometimes referred to as a “probe”) that is tailored to the specific genetic variants(s) involved and other identifying genetic markers. If the patient or a doctor wishes, PGT-A can be completed concurrently with PGT-M. Performing PGT-M before embryo transfer can significantly reduce the risk of having a child with a specific genetic disorder.